At hospitals around Pennsylvania, there are now fewer available intensive care unit beds than at any point since the start of the COVID-19 pandemic, according to data from the Pennsylvania Health Department.
Intensive care units, also known as critical care units, have special resources, such as ventilators, and more staff per patient, than other areas of the hospital.
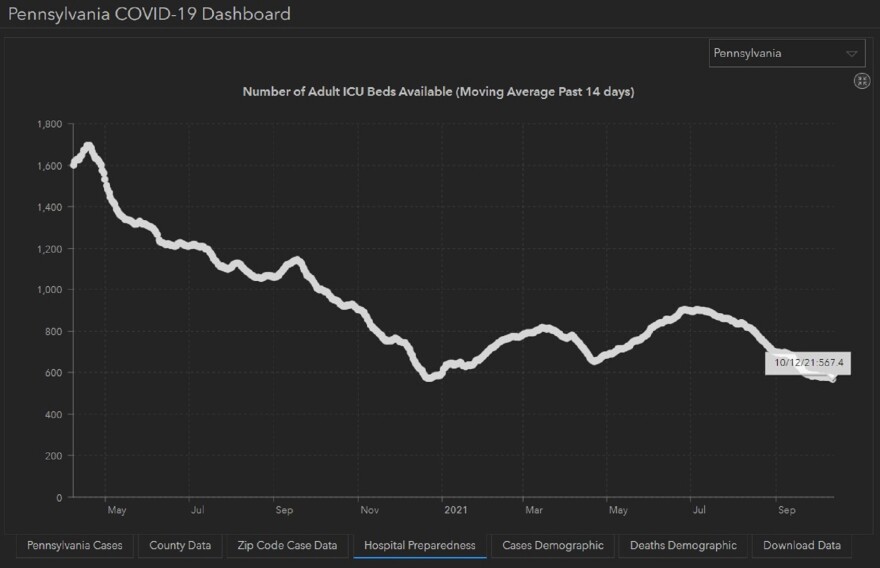
As of Oct. 12, about 567 intensive care unit beds were free for use. During the first surge in April 2020, there were never fewer than 1,600 available beds.
The number of remaining ICU beds have been declining since summer — when daily COVID-19 cases hovered around 190. Since then, average daily case rates have increased 2,270% and are at levels comparable to November 2020 and April 2021.
Department of Health spokeswoman Maggi Barton noted that there are fewer beds available now than during last winter, a concerning trend.
“We know the delta variant is highly transmissible and dangerous to the unvaccinated,” Barton said. “As delta currently represents 98 percent of cases sequenced for variants, we know this variant is playing a role in the increases in cases across our communities.”
Barton noted that about 25% of the nearly 3,000 people hospitalized with COVID-19 are in intensive care units.
While there has been a recent rise in vaccinated people hospitalized with COVID-19, Barton emphasized that “the vaccine continues to be highly effective against the COVID-19 virus, especially serious illness, hospitalization and death.”
The virus isn’t the only factor, said Harrisburg-based infectious disease specialist Dr. Jonathan Goldman at University of Pittsburgh Medical Center.
Goldman said a few things are going on: The delta variant is very infectious. Health care staff shortages are making it harder to move people out of the hospital. And he is seeing patients who have put off going to the doctor for all sorts of illnesses now showing up needing acute care.
“So for example, I do infectious disease, so we’re seeing a lot of people with severe diabetic infections, and I think that some of these are a result of not getting as much care last year.”
These so-called “delay of care” hospitalizations are also playing a role at MIlton S. Hershey Medical Center, according to Dr. Duane Williams, medical director of patient throughput.
The hospital has “several specialty ICUs,” Williams said in an email, and specialized beds for patients with heart, brain and vascular issues are in high demand.
At UPMC Harrisburg, Goldman said there’s one more factor at play as well: doctors are quicker to give people more treatment.
“We clearly have fewer COVID patients than at the height of the pandemic last winter. The issue is really that we’re now, instead of seeing people who are older, sicker, we’re seeing people who are younger, and healthier. And so some are getting more aggressive care.”




